Week 9:
Writing COVI-SWA and the Full Whipple with Reconstruction
August 4, 2021

Olivia, Dr. St Louis, and I at this week’s Journal Club
Week 8 was devoted to quite a bit of shadowing and actually getting to write the COVI-SWA study methods, introduction, and results in sections. In journal club, we discussed a publication that delved into the neurological mechanisms underlying the synaptic homeostasis hypothesis. In addition to writing COVI-SWA, we began creating box plots on R Studio comparing different factors that could affect our data, such as if the participant had a psychiatric diagnosis, with our dependent variable: the chin bilateral any muscle activity REM sleep without atonia (RSWA) metric for which it seems there is a significant difference between our COVID-19 positive participants and control participants. While scoring the participant sleep studies, it was dubious whether we would find a significant difference in any RSWA metric because we were blinded to the participant’s assigned groupings: control or COVID-positive. Finding a positive result could have implications provocative for future study of COVID-19 and its neurological manifestations. Could the SARS-CoV-2 neurological mechanism affect the REM atonia control center, the locus coeruleus, in the brainstem? Could SARS-CoV-2 create a temporary or permanent form of RBD that may or may not phenoconvert to an overt synucleinopathy like Parkinson’s disease (PD), dementia with Lewy bodies (DLB), or multiple system atrophy (MSA)? We have no idea! But jumping off from this data could give us a much clearer picture of both RSWA and SARS-CoV-2 neurological mechanisms as well as how they intersect. We have a very unique chance to delve into studying virology, neurobiology, and immunology altogether with COVI-SWA. Writing sections of it has been enlightening so far, and I can’t wait to work on it more next week, my last week at Mayo Clinic.

Dr. Hieken, breast clinic nurse Marsha, and I
I had the pleasure of shadowing Dr. Tina J. Hieken, a surgical oncologist specializing in breast cancer and melanoma. I shadowed her in the clinic, where we saw many patients with ductile carcinoma in situ (DCIS), invasive lobular cancer, and melanoma. My mother and aunt also had DCIS when I was young, so getting to see the care for their condition and new science attempting to combat its prevalence was an amazing experience. Dr. Hieken researches breast cancer and the microbiome by obtaining specimens from her patients with breast cancer who consent in hopes that specific bacteria will correlate with breast cancer in many participants, which could lead to the production and clinical trials of a vaccine that prevents breast cancer. In the OR, I watched Dr. Hieken and her resident performs a right-breast mastectomy on a patient we had seen the day before for DCIS. It can be difficult to locate blood vessels in the breast tissue, and watching Dr. Hieken, and her resident work out a method to circumvent these vessels was highly engaging. Dr. Hieken was very inspiring, supportive, and a great advocate for female empowerment in the field of surgery. Her mentorship as a highly successful and respected female surgeon, a wonderfully warm persona, and an absolute go-getter is invaluable.
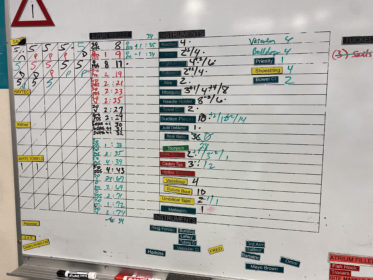
The full Whipple with reconstruction surgery board (picture taken with the permission of the surgical assistants in the absence of any identifying patient information)
I also shadowed the general surgery Trauma Center Critical Care department this week. I got the privilege of witnessing a full Whipple procedure with reconstruction on a patient who had an ATV fall on them that impaled them in the abdomen. Watching Dr. Michael L. Kendrick remove the gall bladder, bile duct, and head of the pancreas of this patient and reconnect the bile duct, stomach, and pancreas to the small intestine for proper digestion and blood flow was a dream of an experience. I was asked to raise and lower the cautery power during the surgery because it was such an all-hands-on-deck situation, with five residents peering over the shoulders of each other on one side of the table to watch Dr. Kendrick perform a once-in-a-year surgery. The surgery involved cautery, staples, and sutures, all counted on the board photo above. The incision was at least a foot long from the bottom of the patient’s ribcage to the height of the patient’s hip bones. It took a total of three hours, after which a resident and an intern closed the incision from the fascia layer first and then began in the middle of the incision, working their way outwards together on the dermis. The experience was fascinating, exciting, hectic, but supremely organized due to the well-oiled machine that is the Mayo Clinic Trauma Center surgery department.

Dr. St Louis and Dr. St Louis’s Minions at our lab pizza party
I closed out the week by shadowing 0ur PI Dr. St Louis, in a clinic with REM Sleep Behavior Disorder (RBD), narcolepsy, and restless leg syndrome (RLS) patients. This observation was equally fascinating, as I could finally apply what we have been working on in the lab all summer to a clinical setting. The RBD patient was especially relevant and shared many vivid details about the disorder with us. This was very enlightening as a demonstration of the real-life consequences this disorder has and the actuality of how it phenoconverts in most patients to a full-blown synucleinopathy like PD. Getting to see Dr. St Louis in the clinic also showed me a different side of him as a physician. When he talks to patients who all have their own stories and struggles, he makes sure to advocate for and explore their lives as a whole. I appreciated his never-ending optimism in a field as difficult as neurology, which contains many chronic illnesses. I hope to reflect his optimism in my future career, hopefully in a clinical setting as he does as well.

Gwen Paule is a chemistry major from Saint Paul, Minnesota
PreviousWeek 8: Finalizing COVI-SWA Preliminary Data
NextWeek 10: Finalizing COVI-SWA Results: The Bittersweet Goodbye
